Lateral Foot Pain - Cuboid Syndrome Part 1
- Dr. Brian Abelson DC
- Jul 3, 2024
- 6 min read
Updated: Aug 12, 2024

Cuboid Syndrome is a common yet often overlooked cause of pain on the outer side of the foot. Despite its prevalence, many healthcare professionals are unfamiliar with the condition, also known as subluxated cuboid, dropped cuboid, cuboid fault syndrome, or lateral plantar neuritis.
Around 7% of people develop Cuboid Syndrome following an ankle sprain, with the incidence rising to 17% among ballet dancers and other athletes. Essentially, Cuboid Syndrome occurs when the cuboid bone shifts out of its normal position, causing it to become stuck and restricting its movement, leading to discomfort and pain.
Our Success Rate is 90%
We are 90% effective in reducing pain and enhancing function in treating Cuboid Syndrome, underscoring the effectiveness of our multimodal, interdisciplinary approach, which focuses on pain relief and restoring optimal foot function.
Article Index

Symptoms of Cuboid Syndrome
Cuboid Syndrome symptoms are often mistaken for an ankle sprain, leading to misdiagnosis or oversight. The pain can be intermittent or constant, appearing suddenly or gradually. Key symptoms include:
Pain that intensifies during the toe-off phase of walking or upon impact.
Lateral foot pain between the calcaneocuboid joint and the fourth and fifth cuboid metatarsal joints.
Tenderness along the lateral side of the foot, the peroneus longus tendon, or around the cuboid bone.
What Causes Cuboid Syndrome?
The causes of Cuboid Syndrome vary. Runners and dancers, particularly ballet dancers, are more susceptible to this injury due to the repetitive impact of their activities. As previously mentioned, Cuboid Syndrome is often associated with ankle inversion sprains, which are among the most common injuries for runners and dancers.

Certain factors frequently emerge when examining the medical history or assessing patients with Cuboid Syndrome. Some of the primary contributing factors include:
Training on uneven surfaces
A history of repeated ankle sprains
Excessive foot pronation
Insufficient foot support
Utilizing inappropriate orthotic support
Anatomy and Biomechanics
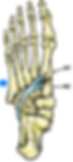
Effectively managing Cuboid Syndrome demands a solid understanding of foot anatomy and biomechanics. The cuboid is one of the seven tarsal bones that support the foot’s structure. These include the cuboid, the medial, intermediate, and lateral cuneiform bones in the midfoot, along with the navicular, talus, and calcaneus (heel bone) in the hindfoot.

The cuboid bone connects to the fourth and fifth metatarsals, forming the tarsometatarsal joint, and joins with the calcaneus (heel bone) to create the calcaneocuboid (CC) joint. Medially, it interacts with the lateral cuneiform and navicular bones, which synchronize their movements during walking.
Proper function of the CC joint is vital for normal walking. This joint allows the cuboid to rotate up to 25 degrees during foot movements like inversion and eversion. The CC joint’s stability comes from its well-aligned surfaces and strong support from tendons and ligaments.

Peroneus Longus Muscle
The peroneus longus muscle plays a crucial role in foot stability. Originating from the upper fibula, it travels down the leg, around the lateral malleolus, through the cuboid groove, and inserts into the base of the first metatarsal and cuneiform.
As it wraps around the cuboid, the peroneus longus forms a supportive sling that enhances foot stability. Together with the tibialis anterior, it supports the medial arch, creating a sling beneath the midfoot.
Biomechanics of the Peroneus Longus:
Aids in foot eversion and ankle plantar flexion
Supports the foot's transverse arches
Stabilizes the lesser tarsals and big toe during subtalar pronation
Clinical Tip: In cases of ankle instability, the peroneus longus may activate differently due to muscle restrictions. Addressing these restrictions is vital to reducing the risk of future injuries, especially for runners.
The Remarkable Cuboid Pulley System
How do these components work together? They create the remarkable Cuboid Pulley System.
At the base of the cuboid bone, a groove houses the tendon of the peroneus longus muscle, forming a powerful pulley mechanism.
This system boosts the mechanical efficiency of the peroneus longus muscle. As you move from mid-stance to late propulsion while walking, the muscle's contraction generates an eversion torque on the cuboid bone, effectively distributing forces to aid in propulsion.
Research indicates that this force distribution helps shift the load across the forefoot, from the lateral to the medial side of the foot.
Conclusion
Cuboid Syndrome, often mistaken for an ankle sprain, presents with distinct foot pain patterns, particularly during walking. Its prevalence among runners and dancers underscores the need to understand foot anatomy and biomechanics. The Cuboid Pulley System, powered by the peroneus longus muscle, plays a key role in foot stability and force distribution. Recognizing the importance of the CC joint and the coordination between the cuboid and navicular bones is crucial for effective treatment and prevention.
In the next part of "Lateral Foot Pain - Cuboid Syndrome," we'll dive into examination procedures, treatment strategies, and rehabilitation techniques to manage this condition effectively.
References Part 1
Marshall P, Hamilton WG. Cuboid subluxation in ballet dancers. The american journal of sports medicine. 1992 Mar;20(2):169-75.
Davenport KL, Keskula DR. (2014). Managing cuboid syndrome in athletes. Current sports medicine reports, 13(6), 365-9.
Neumann, D. A. (2017). Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation (3rd ed.). Elsevier.
Subotnick SI. (1991). Cuboid syndrome. The American journal of sports medicine, 19(2), 192-4.
Durall, C. J. (2011). Examination and treatment of cuboid syndrome: a literature review. Sports Health, 3(6), 514-519. doi: 10.1177/1941738111417565
Adams, E., Madden, C., & Moley, P. (2015). Cuboid Syndrome. Current Sports Medicine Reports, 14(6), 465-469. doi: 10.1249/JSR.0000000000000214
Jennings J, Davies GJ. Treatment of cuboid syndrome secondary to lateral ankle sprains: a case series. Journal of orthopaedic & sports physical therapy. 2005 Jul;35(7):409-15.
Greiner TM, Ball KA. The calcaneocuboid joint moves with three degrees of freedom. Journal of foot and ankle research. 2008 Sep;1(1):O39.
Forman WM, Green MA: The role of intrinsic musculature in the formation of inferior calcaneal exostoses. Clin Podiatr Med Surg. 1990;7:217-223.
Michaud, Thomas C.. Human Locomotion: The Conservative Management of Gait-Related Disorders (p.123). Newton Biomechanics.
Disclaimer:
The content on the MSR website, including articles and embedded videos, serves educational and informational purposes only. It is not a substitute for professional medical advice; only certified MSR practitioners should practice these techniques. By accessing this content, you assume full responsibility for your use of the information, acknowledging that the authors and contributors are not liable for any damages or claims that may arise.
This website does not establish a physician-patient relationship. If you have a medical concern, consult an appropriately licensed healthcare provider. Users under the age of 18 are not permitted to use the site. The MSR website may also feature links to third-party sites; however, we bear no responsibility for the content or practices of these external websites.
By using the MSR website, you agree to indemnify and hold the authors and contributors harmless from any claims, including legal fees, arising from your use of the site or violating these terms. This disclaimer constitutes part of the understanding between you and the website's authors regarding the use of the MSR website. For more information, read the full disclaimer and policies in this website.
DR. BRIAN ABELSON, DC. - The Author

With over 30 years of clinical practice and experience in treating over 25,000 patients with a success rate of over 90%, Dr. Abelson created the powerful and effective Motion Specific Release (MSR) Treatment Systems.
As an internationally best-selling author, he aims to educate and share techniques to benefit the broader healthcare community.
A perpetual student himself, Dr. Abelson continually integrates leading-edge techniques into the MSR programs, with a strong emphasis on multidisciplinary care. His work constantly emphasizes patient-centred care and advancing treatment methods. His practice, Kinetic Health, is located in Calgary, Alberta, Canada.

Join Us at Motion Specific Release
Enroll in our courses to master innovative soft-tissue and osseous techniques that seamlessly fit into your current clinical practice, providing your patients with substantial relief from pain and a renewed sense of functionality. Our curriculum masterfully integrates rigorous medical science with creative therapeutic paradigms, comprehensively understanding musculoskeletal diagnosis and treatment protocols.
Join MSR Pro and start tapping into the power of Motion Specific Release. Have access to:
Protocols: Over 250 clinical procedures with detailed video productions.
Examination Procedures: Over 70 orthopedic and neurological assessment videos and downloadable PDF examination forms for use in your clinical practice are coming soon.
Exercises: You can prescribe hundreds of Functional Exercises Videos to your patients through our downloadable prescription pads.
Article Library: Our Article Index Library with over 45+ of the most common MSK conditions we all see in clinical practice. This is a great opportunity to educate your patients on our processes. Each article covers basic condition information, diagnostic procedures, treatment methodologies, timelines, and exercise recommendations. All of this is in an easy-to-prescribe PDF format you can directly send to your patients.
Discounts: MSR Pro yearly memberships entitle you to a significant discount on our online and live courses.
Integrating MSR into your practice can significantly enhance your clinical practice. The benefits we mentioned are only a few reasons for joining our MSR team.
