Mindfulness: In an Age of Distraction
- Dr. Brian Abelson
- 6 minutes ago
- 12 min read
The Modern Attention Crisis

We are living in an era of engineered distraction.
Smartphones, notifications, and constant digital input have normalized fragmented attention. Many people believe they are multitasking efficiently, but cognitive science tells a different story. Humans do not truly multitask. We task-switch. Each switch requires the brain to disengage one network of activity and activate another. This transition carries a measurable cognitive cost, increasing mental fatigue and reducing performance accuracy.
In a well-known study, heavy media multitaskers showed diminished attentional control and greater vulnerability to distraction compared to light multitaskers (Ophir, Nass & Wagner, 2009). In other words, chronic divided attention appears to weaken the very neural systems required to filter irrelevant information.
Attention is not just a psychological preference. It is a biological process that shapes neural architecture through neuroplasticity, the brain’s ability to strengthen circuits that are repeatedly activated. What we practice, we reinforce. Over time, habitual distraction may consolidate shallow processing while eroding sustained focus.
This concern is particularly important in childhood and adolescence, when executive control networks responsible for impulse regulation and emotional stability are still maturing. High-intensity digital stimulation during sensitive developmental windows has been associated with difficulties in sustained attention and self-regulation (Christakis et al., 2018).
The consequences extend beyond productivity. Attention influences memory consolidation, emotional regulation, and stress responsiveness. It determines whether we react impulsively or respond deliberately.
In a culture that fragments focus, the deliberate training of attention is no longer optional. It is foundational.
What Mindfulness Actually Trains
Mindfulness is frequently mistaken for relaxation, positive thinking, or an attempt to “empty the mind.” It is none of these. At its core, mindfulness is the deliberate training of attention.
More precisely, it strengthens three interrelated capacities: attentional stability, meta-awareness, and response inhibition.
Attentional stability refers to the ability to sustain focus on a chosen object, such as the breath or bodily sensation, without being carried away by distraction. When attention drifts, the practitioner notices and gently returns it. This repetition is not failure; it is the training stimulus. Each return reinforces neural circuits responsible for cognitive control.
Meta-awareness is awareness of awareness itself. It is the capacity to recognize that the mind has wandered. Without meta-awareness, distraction goes unnoticed. With it, individuals gain the ability to observe thoughts as events in the mind rather than facts that demand immediate reaction.
Response inhibition is the ability to pause before acting. In neurocognitive terms, this involves top-down regulation from frontal brain regions that modulate emotional and impulsive reactions. Mindfulness strengthens this regulatory capacity by repeatedly creating a gap between stimulus and response.
Importantly, mindfulness does not eliminate thought. It alters one’s relationship to thought. Instead of being automatically driven by internal narratives, individuals develop the ability to observe them with reduced reactivity.
This shift may appear subtle, but biologically it is profound. Attention is the gateway to perception, emotion, and behavior. Training attention strengthens the neural systems that govern them.
Mindfulness, therefore, is not passive. It is systematic cognitive conditioning.
Large-Scale Brain Networks and Attention
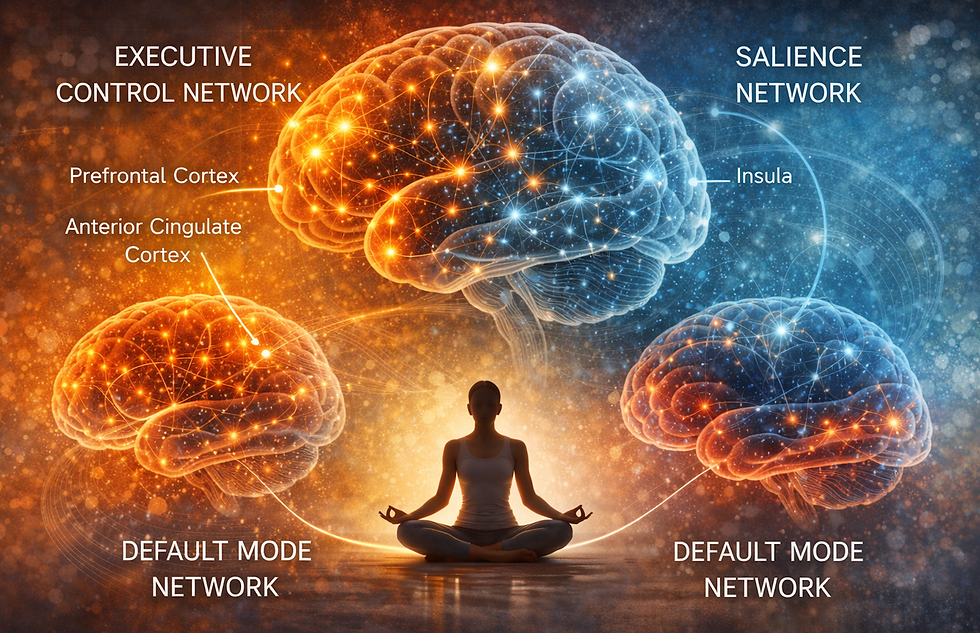
To understand how mindfulness reshapes the brain, it is helpful to think in terms of networks rather than isolated structures. The brain operates through coordinated systems, groups of regions that activate together to perform specific functions. Mindfulness appears to influence several of these large-scale networks in measurable ways.
One of the most important is the Executive Control Network, anchored in regions of the prefrontal cortex and the anterior cingulate cortex. The prefrontal cortex, located behind the forehead, is responsible for planning, decision-making, impulse control, and sustained attention. The anterior cingulate cortex plays a key role in monitoring conflict, detecting errors, and redirecting attention when the mind wanders. Neuroimaging studies have shown structural thickening and enhanced functional connectivity in these regions among mindfulness practitioners, changes associated with improved cognitive regulation (Lazar et al., 2005; Tang et al., 2010).
A second system is the Salience Network, which includes the insula, a region deeply involved in interoception, the perception of internal bodily signals such as heartbeat, breath, and visceral sensation. The salience network helps determine what deserves attention, whether an external stimulus or an internal sensation. Strengthening this network enhances self-awareness and emotional regulation.
Finally, mindfulness influences the Default Mode Network (DMN), a system active during self-referential thinking, mind-wandering, and internal narrative. Excessive DMN activity has been linked to rumination and anxiety. Research suggests mindfulness reduces maladaptive activation within this network and improves the ability to disengage from repetitive self-focused thought (Hölzel et al., 2011; Andrews-Hanna et al., 2021).
Taken together, these changes reflect a shift from automatic narrative processing toward deliberate attentional control. The brain becomes less reactive and more regulated, less scattered and more coherent.
Mindfulness does not quiet the brain by suppression. It refines how networks communicate.
Stress Regulation and the HPA Axis

Attention does not operate in isolation from physiology. How we direct attention influences one of the body’s most powerful regulatory systems: the hypothalamic-pituitary-adrenal axis, commonly called the HPA axis.
The HPA axis is a communication loop between the brain and the adrenal glands. When the brain perceives threat, the hypothalamus signals the pituitary gland, which then instructs the adrenal glands to release cortisol and adrenaline. In short bursts, this response is adaptive. It sharpens focus, mobilizes energy, and prepares the body for action.
The problem arises when stress becomes chronic. Persistent activation of the HPA axis disrupts normal cortisol rhythms. Under healthy conditions, cortisol rises in the morning to promote alertness and gradually declines toward evening to support sleep. Chronic stress can flatten this rhythm, leaving individuals simultaneously wired and fatigued. Dysregulation of this system has been associated with hypertension, metabolic syndrome, impaired immune defense, insomnia, and accelerated biological aging (Miller et al., 2007; McEwen & Akil, 2020).
Mindfulness appears to recalibrate this system rather than suppress it. Clinical studies show reductions in cortisol levels and improved parasympathetic activation following regular mindfulness practice (Pascoe et al., 2017). The parasympathetic nervous system, often described as the “rest-and-digest” branch, counterbalances the fight-or-flight response. When parasympathetic tone improves, heart rate variability increases, sleep stabilizes, and recovery processes strengthen.
Importantly, mindfulness does not eliminate stressors. It alters perception and reactivity. By repeatedly practicing non-reactive awareness, individuals reduce unnecessary amplification of stress signals. The HPA axis becomes less prone to chronic overactivation.
Health depends on rhythm. Mindfulness helps restore it.
Inflammation and Immune Modulation

Stress does not remain confined to the brain. It leaves biochemical fingerprints throughout the body, particularly within the immune system.
When the HPA axis is chronically activated, inflammatory pathways become upregulated. Inflammation is not inherently harmful; it is a protective response designed to eliminate pathogens and repair tissue. However, when inflammatory signaling remains elevated in the absence of infection or injury, it contributes to long-term disease risk. Elevated markers such as C-reactive protein (CRP) and nuclear factor kappa B (NF-κB), a transcription factor that regulates inflammatory gene expression, have been linked to cardiovascular disease, metabolic disorders, autoimmune conditions, and accelerated aging (Creswell et al., 2012).
Psychoneuroimmunology, the study of interactions between psychological processes, the nervous system, and immune function, provides a framework for understanding this connection. Chronic psychological stress amplifies inflammatory signaling. Conversely, practices that reduce stress reactivity can modulate immune responses.
Mindfulness appears to influence this axis of communication. Research suggests regular mindfulness practice is associated with reductions in inflammatory markers, including CRP and NF-κB activity, and improvements in immune cell function, including enhanced regulation of CD4+ T cells, which coordinate adaptive immune responses (Black & Slavich, 2016). These effects are moderate but consistent across multiple studies.
The implication is not that mindfulness replaces medical treatment. Rather, it modifies the internal environment in which disease risk develops. By reducing unnecessary inflammatory activation and supporting immune balance, mindfulness contributes to physiological resilience.
Attention, in this sense, becomes immunologically relevant.
Mindfulness and Cellular Aging

Aging is often measured in years, but it is also written into our cells.
At the ends of each chromosome lie structures called telomeres, protective caps composed of repetitive DNA sequences. They function much like the plastic tips on shoelaces, preventing genetic material from fraying during cell division. Each time a cell divides, telomeres shorten slightly. Over time, excessive shortening can impair cellular function and contribute to biological aging.
Chronic psychological stress accelerates this process. Elevated cortisol, persistent inflammation, and oxidative stress have all been associated with shortened telomere length (Epel et al., 2004). Individuals exposed to prolonged stress often show signs of accelerated cellular aging compared to less stressed counterparts.
Mindfulness appears to influence this pathway indirectly through stress regulation. Several studies have reported increased activity of telomerase, the enzyme responsible for maintaining and repairing telomeres, among individuals engaged in regular mindfulness practice (Blackburn et al., 2015; Rao et al., 2015). A meta-analysis suggests mindfulness-based interventions are associated with modest but measurable increases in telomerase activity (Schutte & Malouff, 2014).
It is important to interpret these findings cautiously. Mindfulness is not a cellular fountain of youth. The effects observed are moderate and influenced by many variables, including overall lifestyle and health status. However, the consistency of findings suggests that stress modulation may translate into measurable cellular benefits.
The implication is profound: the way we regulate attention and stress may influence aging at the molecular level.
Biology listens to psychological state more closely than we once believed.
Clinical and Practical Implications
The biological effects of mindfulness are not merely theoretical. They translate into measurable clinical relevance.
For practitioners, mindfulness represents a foundational regulatory intervention. In chronic pain, for example, altered activity within the default mode network and heightened amygdala reactivity can amplify suffering beyond tissue damage. Training attentional control helps patients observe pain sensations without immediately layering catastrophic interpretation onto them. This shift can reduce perceived intensity and improve functional outcomes.
In anxiety and trauma-related conditions, strengthening executive control networks enhances top-down modulation of limbic activation, allowing individuals to respond rather than reflexively react. For clinicians themselves, mindfulness has been associated with reduced burnout, improved emotional resilience, and enhanced therapeutic presence.
For the general reader, the implications are equally practical. Improved attentional stability supports deeper work, clearer decision-making, and more meaningful interpersonal connection. Stress regulation improves sleep quality and emotional steadiness. Reduced inflammatory signaling and better autonomic balance contribute to long-term health resilience.
Mindfulness does not replace medical treatment, psychotherapy, or structured rehabilitation. It augments them. By strengthening regulatory systems at multiple levels, cognitive, autonomic, and immune, mindfulness creates a more stable internal environment in which healing and performance can occur.
It is not an alternative intervention. It is a foundational one.
An Exercise You Can Try
Mindfulness does not require extended retreats or complex rituals. It begins with deliberate, consistent practice.
Start with five minutes daily. Sit upright in a quiet space. Allow the eyes to close or soften. Choose a single anchor for attention, most commonly the natural sensation of breathing. Do not attempt to control the breath. Simply observe it as it moves in and out.
Within seconds, the mind will wander. Thoughts, plans, memories, and distractions will arise. This is not a problem; it is the training stimulus. The critical step is noticing that attention has drifted. That moment of recognition, called meta-awareness, is the strengthening phase. Gently return attention to the chosen anchor without self-criticism.
Repeat this cycle throughout the session. Each return reinforces neural circuits involved in cognitive control and emotional regulation.
Consistency matters more than duration. Five focused minutes daily is more effective than occasional longer sessions. Over time, attentional stability increases, reactivity decreases, and awareness becomes more continuous.
Like physical conditioning, the benefits accumulate gradually.
Trajectory

Many of the principles explored here form part of a broader, integrated framework presented in my forthcoming book, Trajectory. Chapter 5 focuses specifically on mindfulness, examining how deliberate attention training strengthens cognitive regulation, stabilizes stress physiology, supports immune balance, and influences long-term brain adaptability.
Scheduled for release in late 2026 or early 2027, Trajectory brings together neuroscience, physiology, and practical application into a cohesive, evidence-informed model for optimizing cognitive development, resilience, and overall health across the lifespan.
References
Andrews-Hanna, J. R., Smallwood, J., & Spreng, R. N. (2021). The default network and self-generated thought: Component processes, dynamic control, and clinical relevance. Annals of the New York Academy of Sciences, 1481(1), 29–52.
Black, D. S., & Slavich, G. M. (2016). Mindfulness meditation and the immune system: A systematic review of randomized controlled trials. Annals of the New York Academy of Sciences, 1373(1), 13–24.
Blackburn, E. H., Epel, E. S., & Lin, J. (2015). Human telomere biology: A contributory and interactive factor in aging, disease risks, and protection. Science, 350(6265), 1193–1198.
Christakis, D. A., Ramirez, J. S. B., Ferguson, S. M., Ravinder, S., & Ramirez, J. M. (2018). How early media exposure may affect cognitive function: A review of results from observations in humans and experiments in mice. Proceedings of the National Academy of Sciences, 115(40), 9851–9858.
Creswell, J. D., Irwin, M. R., Burklund, L. J., Lieberman, M. D., Arevalo, J. M. G., Ma, J., & Cole, S. W. (2012). Mindfulness-based stress reduction training reduces loneliness and pro-inflammatory gene expression in older adults: A randomized controlled trial. Brain, Behavior, and Immunity, 26(7), 1095–1101.
Epel, E. S., Blackburn, E. H., Lin, J., Dhabhar, F. S., Adler, N. E., Morrow, J. D., & Cawthon, R. M. (2004). Accelerated telomere shortening in response to life stress. Proceedings of the National Academy of Sciences, 101(49), 17312–17315.
Hölzel, B. K., Carmody, J., Vangel, M., Congleton, C., Yerramsetti, S. M., Gard, T., & Lazar, S. W. (2011). Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Research: Neuroimaging, 191(1), 36–43.
Lazar, S. W., Kerr, C. E., Wasserman, R. H., Gray, J. R., Greve, D. N., Treadway, M. T., & Fischl, B. (2005). Meditation experience is associated with increased cortical thickness. NeuroReport, 16(17), 1893–1897.
McEwen, B. S., & Akil, H. (2020). Revisiting the stress concept: Implications for affective disorders. The Journal of Neuroscience, 40(1), 12–21.
Miller, G. E., Chen, E., & Zhou, E. S. (2007). If it goes up, must it come down? Chronic stress and the hypothalamic–pituitary–adrenal axis in humans. Psychological Bulletin, 133(1), 25–45.
Ophir, E., Nass, C., & Wagner, A. D. (2009). Cognitive control in media multitaskers. Proceedings of the National Academy of Sciences, 106(37), 15583–15587.
Pascoe, M. C., Thompson, D. R., Jenkins, Z. M., & Ski, C. F. (2017). Mindfulness mediates the physiological markers of stress: Systematic review and meta-analysis. Journal of Psychiatric Research, 95, 156–178.
Rao, X., Harrington, L. A., & Muehlenbein, M. P. (2015). Mindfulness and telomere length: A systematic review. Psychoneuroendocrinology, 58, 70–79.
Schutte, N. S., & Malouff, J. M. (2014). A meta-analytic review of the effects of mindfulness meditation on telomerase activity. Psychoneuroendocrinology, 42, 45–48.
Tang, Y. Y., Lu, Q., Fan, M., Yang, Y., & Posner, M. I. (2010). Mechanisms of white matter changes induced by meditation. Proceedings of the National Academy of Sciences, 107(35), 15649–15652.
.
DR. BRIAN ABELSON, DC. - The Author

With over 30 years of clinical experience and more than 25,000 patients treated, Dr. Brian J. Abelson is the creator of Motion Specific Release (MSR), a multidisciplinary assessment and treatment system that integrates biomechanics, fascia science, neurology, manual therapy, exercise rehabilitation, and acupuncture. He is an internationally recognized best-selling author of 10 books and 200+ articles, and has trained healthcare professionals through structured MSR courses and clinical education programs throughout Canada and the United States. Dr. Abelson practices at Kinetic Health in Calgary, Alberta, and continues to develop educational resources focused on long-term function, resilience, and the health trajectory shaped by everyday choices.
For patients, his goal is simple, reduce pain, restore movement, and build long-term independence. For practitioners, MSR provides a practical framework you can integrate directly into daily clinical care.

Why Choose MSR Courses and MSR Pro?
Elevate your clinical practice with Motion Specific Release (MSR) training and MSR Pro, a comprehensive, evidence-informed approach to musculoskeletal assessment and treatment designed to improve diagnostic precision, hands-on skill, and patient outcomes.
MSR proficiency goes far beyond videos and articles. True clinical mastery requires hands-on training, refinement of palpation and force application, and a deeper command of applied anatomy and biomechanics. MSR is a skill-based system built through deliberate practice, real-time feedback, and mentorship, where clinical reasoning and tactile execution come together.
Here’s why practitioners join MSR:
Proven Clinical SystemDeveloped by Dr. Brian J. Abelson, DC, with over 30 years of clinical experience and more than 25,000 patients treated, MSR integrates the most effective components of osseous and myofascial therapies into a cohesive, repeatable framework. The system is grounded in clinical logic and supported by patient outcomes, with a clinic success rate exceeding 90% in decreasing pain and improving function.
Comprehensive, Practical TrainingCourses blend rigorous clinical education with hands-on technique development. You’ll strengthen orthopedic and neurological examination skills while learning targeted myofascial procedures, fascial expansion concepts, and osseous adjusting and mobilization strategies that translate directly into daily practice.
MSR Pro, Your Clinical LibraryAs an MSR Pro subscriber, you gain access to a growing library of 200+ MSR procedures, instructional videos, downloadable and fillable clinical forms, and in-depth practitioner resources that support the full clinical workflow, from intake to reassessment and exercise prescription.
Ongoing Support and UpdatesMSR Pro includes an extensive resource base of 750+ videos, including technique instruction, rehabilitation exercise progression, and clinical application guidance, supported by a large MSK article library and condition-based resources. Content is actively updated and expanded to reflect evolving clinical needs and course development.
A System Built for GrowthMSR is designed to help practitioners think clearly in complex presentations, develop adaptable strategies, and evolve as clinicians. This approach aligns with the broader Trajectory principle, better outcomes are built through the cumulative power of consistent, high-quality clinical decisions.
Unlock your practice’s full potential with MSR Courses and MSR Pro, and join a community of practitioners committed to excellence in musculoskeletal care.
YouTube Channel
Explore Dr. Abelson’s YouTube channel, Kinetic Health Online, with 200,000+ subscribers and 37+ million views.
The channel features a large library of evidence-informed musculoskeletal education, including Motion Specific Release (MSR) procedures that integrate fascial-based concepts, manual therapy, movement science, and select Traditional Chinese Medicine (TCM) principles.
You’ll also find:
70+ essential physical examination videos
MSK condition tutorials and clinical education content
Hundreds of mobility, strengthening, and rehab exercise demonstrations
A dedicated Yang Style Tai Chi playlist, reflecting Dr. Abelson’s decades of teaching experience
Disclaimer:
The content on the MSR website, including articles and embedded videos, is provided for educational and informational purposes only and is not a substitute for individualized medical advice, diagnosis, or treatment. MSR techniques require appropriate professional training; do not attempt or apply these procedures unless you are properly trained and licensed where applicable. By accessing this content, you assume full responsibility for your use of the information, and to the fullest extent permitted by law, the authors and contributors disclaim liability for any loss, injury, or damages arising from its use.
This website does not establish a healthcare provider–patient relationship. If you have a medical concern, consult a qualified, licensed healthcare professional. This website is intended for adults and is not directed to individuals under 18. The MSR website may include links to third-party sites; we do not control and are not responsible for the content, accuracy, or practices of external websites.
By using this website, you agree to indemnify and hold harmless the authors and contributors from any claims, liabilities, and legal fees arising from your use of the site or violation of these terms. For more information, please review the full disclaimer and policies on this website.





Comments