Meniscus Injuries Part 2 - Diagnosis & Acute Stage
- Dr. Brian Abelson DC
- Sep 2, 2024
- 6 min read
Navigating a suspected meniscus injury can be daunting, but a thorough, well-rounded approach can make all the difference. In this second part of our comprehensive guide, we'll explore the critical steps in diagnosing and managing meniscus injuries. We cover everything from detailed physical examinations and diagnostic imaging to interpreting symptoms accurately. Discover the initial actions to take if you suspect a meniscus tear and understand why these steps are vital for your recovery. Whether you're a healthcare professional looking to deepen your expertise or someone experiencing knee pain, join us to learn about the importance of a meticulous approach in addressing meniscus injuries.
Article Index:
Physical Examination for Meniscus Injuries

Conducting a comprehensive physical examination is essential in cases of suspected meniscus injuries. This examination should encompass a detailed history, orthopedic tests, and a neurological assessment. Diagnostic imaging may also play a crucial role in determining the extent of the meniscus injury.
Orthopedic, Neurological and Vascular Testing
The following demonstration videos present common orthopedic, neurological, and peripheral vascular examination tests used in cases of suspected meniscus injuries.

Effective Orthopaedic Testing
This video demonstrates some common orthopedic tests we use to examine our patient's knees.
Lower Limb Neuro Examination
The lower limb neurological examination is part of the overall neurological examination process and is used to assess the motor and sensory neurons which supply the lower limbs. This assessment helps to detect any impairment of the nervous system. It is used both as a screening and an investigative tool.
Peripheral Vascular Examination - Key Points
A peripheral vascular examination is valuable for ruling out signs of vascular-related pathology. The detection and subsequent treatment of PVD can potentially mitigate cardiovascular and cerebrovascular complications. In this video, we review some common procedures we perform in daily clinical practice.
Imaging

X-rays
Although X-rays are not highly effective in diagnosing meniscus injuries, they should still be taken, as they provide valuable information that can help rule out degenerative joint changes, fractures, or pathological processes. Recommended views include an anteroposterior weight-bearing view, posteroanterior 45º flexed view, lateral view, and Merchant Patellar view.

Magnetic Resonance Imaging (MRI)
MRI provides some of the most accurate imaging for meniscus injuries, with an 88% accuracy rate for medial and 92% for lateral meniscal tears. These accuracy levels are comparable to those obtained through a comprehensive physical examination. Research indicates that a thorough physical exam is an equally valuable diagnostic tool and should be used with imaging results.
However, this doesn't mean that MRI should be disregarded. Instead, it suggests that MRI should not be the first line of investigation due to its high costs and that a comprehensive physical examination can yield equivalent diagnostic information.
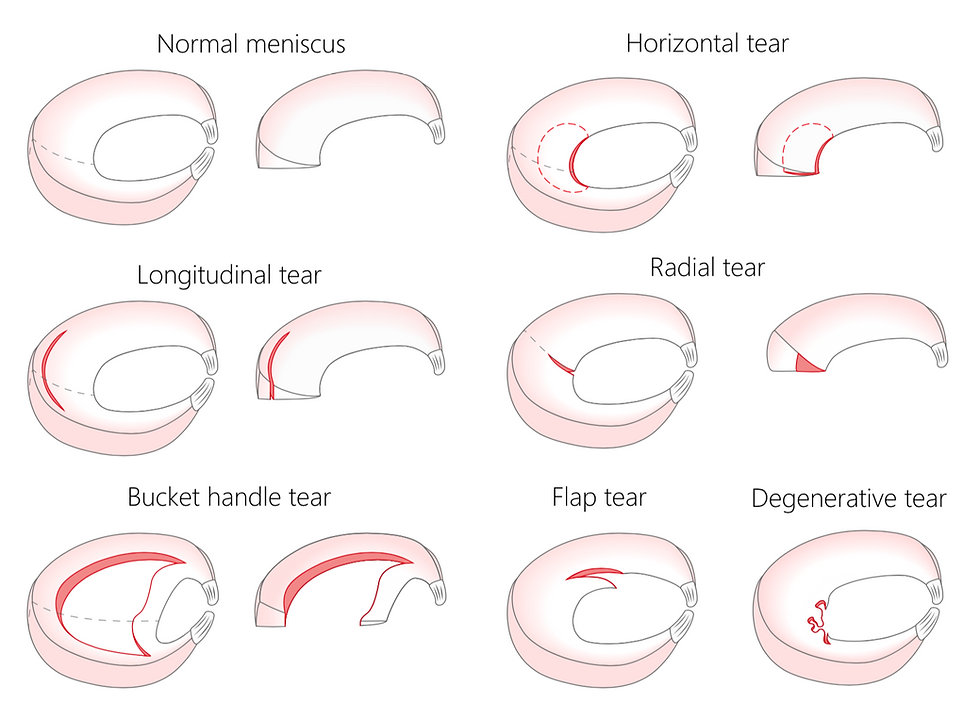
Types of Meniscus Tears
Meniscal tears can be classified into three basic shapes: longitudinal, horizontal, and radial. Complex tears are a combination of these three fundamental shapes. Each tear shape has specific displaced forms:
Longitudinal tear: When displaced, it is known as a "bucket handle tear." This type of tear is one of the most common causes of a locked knee.
Horizontal tear: A displaced horizontal tear is called a "flap tear."
Radial tear: When a radial tear is displaced, it is called a "parrot beak tear" (4).
These classifications help medical professionals better understand the nature of the injury and determine the most appropriate treatment approach. The tear's shape and displacement can impact the healing process and the choice of surgical or non-surgical interventions.
If You Suspect a Meniscus Injury
First and foremost, seek immediate medical attention if you experience any signs of a meniscus tear. It is crucial to determine the severity of the injury.
The extent of your injury will dictate the appropriate strategy for addressing your meniscus tear. Additionally, it is vital to cease all activities that could potentially worsen the knee damage until a medical practitioner has completed their assessment.

Upon Initial Meniscus Injury:
Regardless of the injury's severity, it's crucial to follow the RICE (rest, ice, compression, and elevation) procedure at the onset of a meniscus tear, and here's why:
Rest - Limit stress on the knee to prevent further damage. Use crutches and a neoprene brace to keep the knee locked in extension if needed. Resting allows the injured area to begin the healing process.
Ice – Applying ice to the knee for 20-30 minutes every 2-3 hours helps reduce swelling and inflammation. Cold therapy constricts blood vessels, minimizing pain and discomfort.
Compression - An elastic tensor bandage on your knee helps reduce swelling by limiting fluid accumulation in the injured area. It can be used in conjunction with ice for added benefits.
Elevation—Elevating your knee helps decrease swelling by promoting blood flow back to the heart. Place your knee on a blanket or pillow to keep it elevated and supported.

Clarifying the Meaning of Rest
Depending on the severity of the injury, complete recovery may necessitate resting your knee for several weeks. Initially, you should avoid activities that involve knee flexion. Flexing the knee generates tension in the popliteus and semimembranosus muscles, which are connected to the meniscus, increasing stress in the area.
Clinical Tip: By keeping the injured knee locked and fully extended, you can reduce about 50% of the compressive load on the knee.
Resting the injured leg does NOT mean abstaining from all physical activities. Here's why:
Exercising the lower extremity of the non-injured leg helps maintain overall muscle mass in the injured leg, preventing muscle atrophy in that limb.
Working out the opposite leg leads to neurological crossover, which aids in maintaining muscle strength on the injured side without causing further damage.
Using electrical stimulation, like inferential current, can also help prevent muscle atrophy in the injured leg without adding stress to the meniscus.
Conclusion Part 2
In conclusion, managing a suspected meniscus injury effectively requires a comprehensive approach, blending physical examinations, diagnostic imaging, and symptom interpretation. This guide has emphasized the importance of thorough assessments and initial actions to ensure proper care and recovery. By understanding the types of meniscus tears and the steps to take when an injury occurs, healthcare professionals and individuals can make informed decisions to facilitate healing.
Combining clinical expertise with practical steps like the RICE protocol can significantly impact recovery outcomes, ultimately promoting long-term knee health and functionality.
Note: References for "Knee Pain - Meniscus Injuries are at the end of Part 3.
Disclaimer:
The content on the MSR website, including articles and embedded videos, serves educational and informational purposes only. It is not a substitute for professional medical advice; only certified MSR practitioners should practice these techniques. By accessing this content, you assume full responsibility for your use of the information, acknowledging that the authors and contributors are not liable for any damages or claims that may arise.
This website does not establish a physician-patient relationship. If you have a medical concern, consult an appropriately licensed healthcare provider. Users under the age of 18 are not permitted to use the site. The MSR website may also feature links to third-party sites; however, we bear no responsibility for the content or practices of these external websites.
By using the MSR website, you agree to indemnify and hold the authors and contributors harmless from any claims, including legal fees, arising from your use of the site or violating these terms. This disclaimer constitutes part of the understanding between you and the website's authors regarding the use of the MSR website. For more information, read the full disclaimer and policies in this website.
DR. BRIAN ABELSON, DC. - The Author

With over 30 years of clinical practice and experience in treating over 25,000 patients with a success rate of over 90%, Dr. Abelson created the powerful and effective Motion Specific Release (MSR) Treatment Systems.
As an internationally best-selling author, he aims to educate and share techniques to benefit the broader healthcare community.
A perpetual student himself, Dr. Abelson continually integrates leading-edge techniques into the MSR programs, with a strong emphasis on multidisciplinary care. His work constantly emphasizes patient-centred care and advancing treatment methods. His practice, Kinetic Health, is located in Calgary, Alberta, Canada.

Join Us at Motion Specific Release
Enroll in our courses to master innovative soft-tissue and osseous techniques that seamlessly fit into your current clinical practice, providing your patients with substantial relief from pain and a renewed sense of functionality. Our curriculum masterfully integrates rigorous medical science with creative therapeutic paradigms, comprehensively understanding musculoskeletal diagnosis and treatment protocols.
Join MSR Pro and start tapping into the power of Motion Specific Release. Have access to:
Protocols: Over 250 clinical procedures with detailed video productions.
Examination Procedures: Over 70 orthopedic and neurological assessment videos and downloadable PDF examination forms for use in your clinical practice are coming soon.
Exercises: You can prescribe hundreds of Functional Exercises Videos to your patients through our downloadable prescription pads.
Article Library: Our Article Index Library with over 45+ of the most common MSK conditions we all see in clinical practice. This is a great opportunity to educate your patients on our processes. Each article covers basic condition information, diagnostic procedures, treatment methodologies, timelines, and exercise recommendations. All of this is in an easy-to-prescribe PDF format you can directly send to your patients.
Discounts: MSR Pro yearly memberships entitle you to a significant discount on our online and live courses.
Integrating MSR into your practice can significantly enhance your clinical practice. The benefits we mentioned are only a few reasons for joining our MSR team.






Comments